Opioid abuse is at epidemic proportions in the US today.
Contrary to popular imagery, the opioid addict could be your co-worker, neighbor or even your own child.
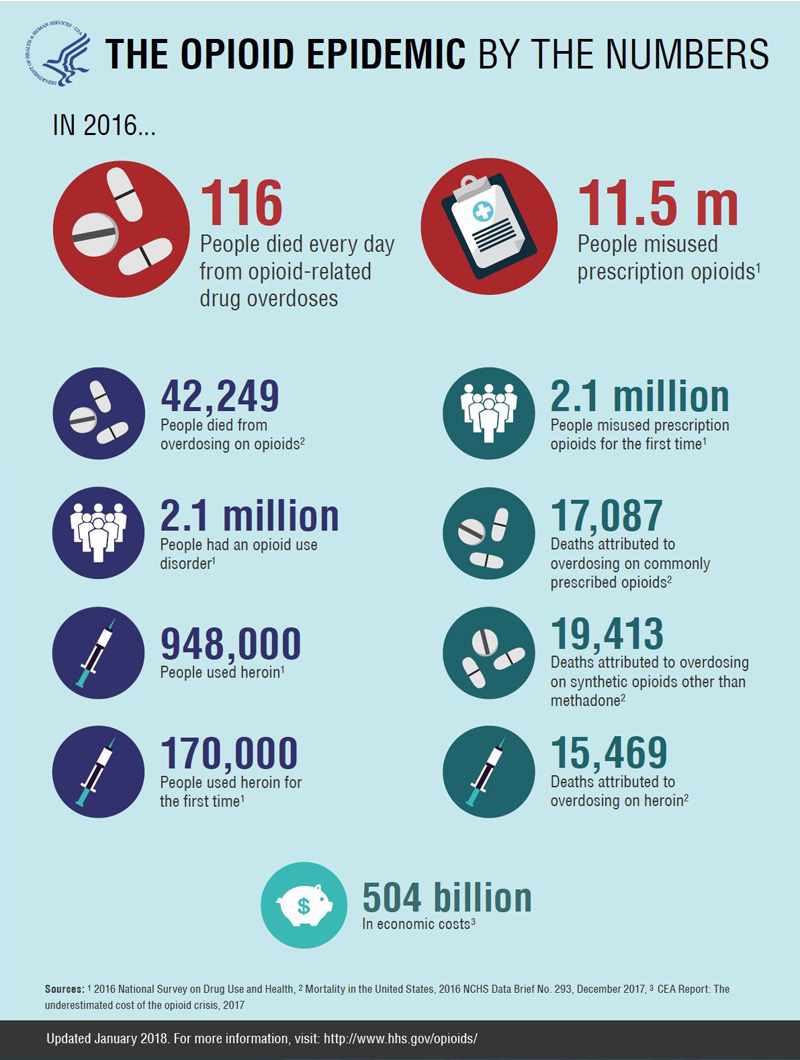
11.5 million Americans aged 12 and over misused a prescription pain reliever in the past year ― with hydrocodone, oxycodone, and codeine products being the most commonly reported.
The most common source of pain relievers in the 2016 NSDUH [National Survey on Drug Use and Health] was “a friend or relative” (53%) [who, in all likelihood, got them from a physician who gave them a prescription]. “A physician’s prescription” was the second most common source, reported by approximately 35% of respondents.
In January 2018, the FDA took the unprecedented step of announcing two plans to help reduce opioid abuse.
The FDA followed this by obtaining voluntary agreement from some opioid drug manufacturers to change their packaging to smaller doses, particularly for immediate-release drugs. There is early evidence that smaller packs will encourage the prescribing of shorter term doses and closer monitoring by the health care provider.
How did this epidemic happen?
How do perfectly normal, rational, good people with families, jobs and friends, suddenly find they are addicted to opioid pain medication? How do teenagers who have never taken an opioid medication, are totally against drug use, but take one prescription – and become addicted?
One hundred million Americans suffer from common chronic pain conditions; fewer than half of Americans undergoing surgery report adequate pain relief; and 60% of Americans visiting the emergency department with acute painful conditions receive pain medication (things like hydrocodone, oxycodone, and codeine).
You may be more familiar with hydrocodone as: Vicodin, Anexsia, Lortab, Hydrogesic, Norco, Zydone, Vicoprofen, Verdocet, among others. Oxycodone is known as: Oxycontin, Percocet, Percodan, Roxicodone, Roxicet, among others. Codeine is also known as: Tylenol with codeine. Hydromorphone is Dilaudid. Ask your physician, dentist or pharmacist if you are not sure if your prescription contains an opioid.
Health-care professionals can begin to stem the tide of this epidemic by finding non-opioid means for managing pain, both chronic and acute (such as post-surgical). They also must learn to recognize levels of pain and how to recognize specific risk factors for a patient who may abuse pain medication, particularly if treatment cannot provide adequate relief from chronic pain. They should consider referring a patient out to a pain specialist, if necessary.
It is also very important for health-care professionals be knowledgeable about the basic elements of addiction medicine and be familiar with the terminology, definitions, neurobiology, and neuropharmacology of opioids, as they apply to treatment with these drugs in their practices.
Risks prescribers must be aware of –
For example, in report from the Centers for Disease Control and Prevention (CDC), they suggest that authorization of a second opioid prescription doubles the risk for opioid use by that patient 1 year later and that increased awareness of this trend is needed among prescribers, pharmacists and persons managing benefit plans – and might deter over-prescribing of opioids.
They should also be aware that the risks for chronic opioid use increase with each additional day supplied, presenting an excellent reason to evaluate initial prescriptions with an early discussion with the patient on how to manage pain early in the prescription process, as well as advising him or her of the dynamics and risks of opioid addition and how to avoid it.
How often and to whom are opioid pain killers prescribed?
In an analysis of 79.5 million prescriptions for opioid pain medications (85% of which were for hydrocodone- and oxycodone-containing products), they were dispensed as follows:
0-9 years 0.7% (0.6 million)
10- 29 years 11.7% (9.3 million)
40-59 years, 45.7% (36.4 million)
Primary care physicains accounted for 29% (22.9 million)
Internists, 14.6% (1.6 million)
Dentists, 8% (6.4 million)
Orthopedic surgeons, 7.7% (6.1 million)
For patients aged 10-19, dentists were the main prescribers 30.8% (.7 million), followed by,
primary care 13.1% (1.3 million) and emergency physicians 12.3% (0.3 million).
In this study, across all ages and specialties, 56.4% (44.8 million) of opioid prescriptions were dispensed to patients who had already filled another prescription within the past month. (6)
Here is an excerpt from the FDA “Blue Print” (see link given above):