World Oral Health Day
Recent studies show that treating periodontal disease can substantially reduce certain chronic diseases AND the costs of treating them.
The authors of the below-referenced study—and the people whose data they analyzed—provide us with convincing evidence that DENTISTS AND PHYSICIANS who understand and address the oral-systemic connection can substantially reduce the chronic disease burden in the US and the world – and the direct and indirect costs related to those conditions.
Let me explain…
Visiting the dentist could not only help fight some of the leading causes of death, it could also significantly reduce health-care costs.
A study was published in the American Journal of Preventive Medicine from the University of Pennsylvania School Of Dental Medicine. Coauthors from medical and dental insurance companies, which provided the data, found that people with some of the most prevalent chronic conditions who had their periodontal disease treated…
1) Racked up significantly lower medical bills AND
2) Had significantly fewer hospitalizations over a 4-year period than those who didn’t.
These authors looked at 4 chronic health conditions, three of which are leading causes of death in the US and the world.
- Coronary artery disease (heart disease)- #1 (US and the world)
- Cerebral vascular disease (stroke) – #3 (this is combined as #1 in the world)
- Type-2 diabetes – #6 (#8 in the world)
- Rheumatoid arthritis (mortality rates tied to cardiovascular health)
They studied a population of 338,891 people with medical AND dental insurance who ALSO had diagnosed periodontal disease, over a period spanning 2005-2009. To keep things more objective, one criterion for analysis was no periodontal treatment during the pre-study year, 2004.
Comparing the 2 outcomes:
They compared the 2 outcomes
1: total medical costs
2: total hospital admissions—irrespective of cause)
between those people who did – and those who did NOT – get their periodontal disease treated beginning in 2005, up through 2009.
The results showed significantly lower annualized costs AND hospital admissions among the periodontally treated patients for 3 out of the 4 conditions—only rheumatoid arthritis showed a drop that wasn’t statistically significant (meaning the drop could’ve happened by chance).
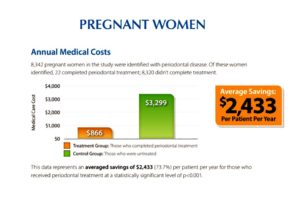
They looked at Pregnancy outcomes…
On a more positive note, they also looked at data from women in this group with periodontal disease who had a first or a second pregnancy during 2005-2009—but had NONE of the 4 chronic diseases—and computed differences in medical costs for atypical medical visits only (hospital admissions weren’t analyzed). The biggest overall cost reductions occurred among women who had a first pregnancy AND got their gum disease treated (a whopping 73.7% annual drop).
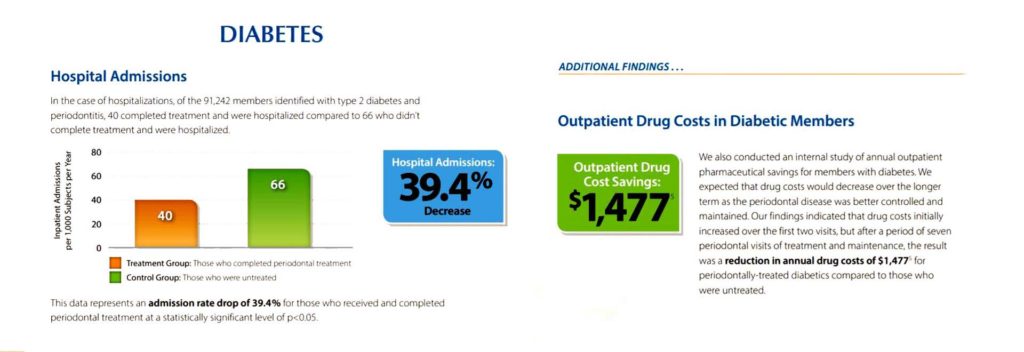
And they looked at outcomes for diabetic patients and those with cerebrovascular disease (stroke)…
The next-biggest cost savings occurred among gum-conscious people with diabetes (40.2% annual drop) and cardiovascular disease – stroke (40.9% annual drop).
These 2 conditions also saw big annual drops in hospital admissions (39.4% and 21.2%, respectively).
And here are the statistics for cerebrovascular disease (stroke)…
And they looked at coronary artery patient outcomes…
BUT…those with coronary artery disease also saw a whopping 28.6% yearly drop in hospital admissions. Along with this was a less spectacular—but still statistically significant—10.7% yearly drop in their medical cost totals, if they had a periodontal treatment regimen during those 4 years.
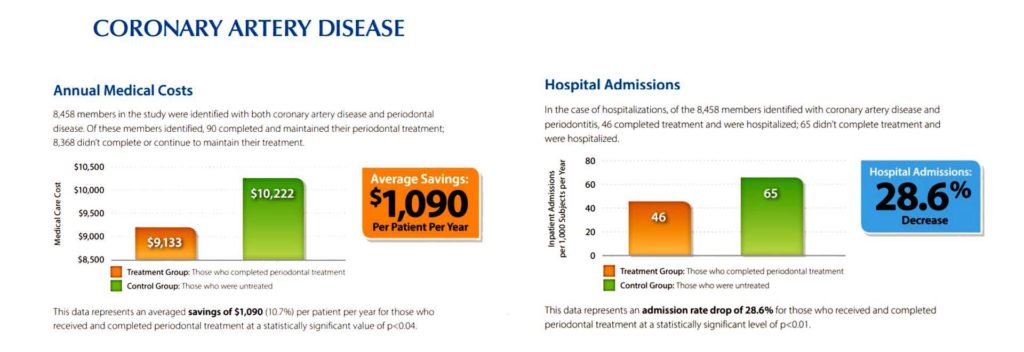
I highlight this last number because heart disease is probably THE systemic condition most people understand IS connected to oral health. As the leading cause of death in the US and the world—heart disease is something we should all be focused on reducing. So this number should resonate…even with folks who DON’T have heart disease.
These study results should provide an incentive to patients
These study results should provide an incentive to patients to keep their teeth and gums healthy. And if they DO have periodontal disease, to get it treated by professionals.
Dentistry has more capabilities today than ever before to heal and regenerate gums and supporting bone.
Please share this email with friends, family, patients and clinicians who can benefit from seeing these study results and leave me a comment below…
Bottom line, getting regular dental care can save your life – and your wallet!
Here is some of what the authors (see References) have to say about their findings:
Implications of Disease Management and Prevention: “If evidence continues to accumulate that an oral–systemic health link not only exists but also can be exploited to improve general health, two important consequences can be expected. Clinically, it would be logical for assessment and treatment of periodontal disease to be routinely considered in the management of specific medical conditions. Scientifically, further research, clinical and otherwise, could be better focused on the underlying pathways and causal factors.”
“Conclusions: Preventive dental care is strongly associated with significant savings for diabetes and CAD patients, and such savings were highest for diabetes + CAD patients, followed by patients with only CAD and only diabetes. Practical Implications: Health plans should include dental coverage in their benefits package and incentivize adherence with preventive dental care to improve health and lower costs for enrollees with diabetes and CAD.”
“Conclusions: Any improvement in the control of diabetes and/or periodontal disease has the potential to improve significantly the quality of life in diabetic subjects.”
References:
All slides from United Concordia Dental white paper “The Mouth – The Missing Piece to Overall Wellness and Lower Medical Costs”.
https://www.ajpmonline.org/article/S0749-3797%2814%2900153-6/fulltext
https://www.aegisdentalnetwork.com/cced/2022/03/association-between-preventive-dental-care-and-healthcare-cost-for-enrollees-with-diabetes-or-coronary-artery-disease-5-year-experience
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4499526/


As far as I know, these graphics are not available as posters, etc. since they are part of a White Paper. You might try contacting United Concordia Dental who produced the White Paper -The Mouth – The Missing Piece to Overall Wellness and Lower Medical Costs. http://www.UnitedCondordia.com.
Very interesting study! Are these graphics available for display in office , or for public education purposes?